Eczema (Atopic dermatitis) can affect people of all ages and can cause quite a bit of misery. In order to get rid of eczema, you need to know more about the cause, diagnosis and symptoms of eczema and we will also suggest some treatments to manage it.
What is Eczema?

Eczema is a term used synonymously with atopic dermatitis. Eczema can affect people of all ages and can cause quite a bit of misery.
It is characterized by dry, itchy, scaly and red skin. Eczema has been found to be closely linked to the development of asthma and allergic rhinitis (nose allergy) in individuals with genetic predisposition towards allergy conditions.
What is the main cause of Eczema?
The exact cause of eczema is not completely well understood. It may result from an interplay between genetic (hereditary) and environmental factors.
How to diagnose?
There is no test for eczema. Diagnosis is usually based on a person’s medical history and physical examination of the skin. A personal or family history of allergy and early onset of symptoms at a young age may also help support and confirm the diagnosis.
What are the symptoms?
Intense skin itching, redness, skin flaking and small bumps are typical symptoms of eczema, although the exact presentation may vary from person to person.

- In babies, rashes tend to form at the front of the legs, outer part of the elbows, cheeks and scalp.
- In older children and adults, the rash is usually located at the side of the neck, elbow creases and the back of knees. For adults, flexure areas such as the elbows and knees are more commonly affected. With time, the inflamed skin may darken and become thick.
Does Eczema ever go away?
Since eczema normally develops in childhood, some people can get rid of it when they grow up. But for the majority, it is a lifelong inflammatory skin condition that cannot be cured.
Having said that, symptoms can be controlled with moisturizers, self-care measures and medications.
What are the top Eczema triggers?
Factors that aggravate eczema include:
- Extreme temperatures such as very hot or cold weather
- Dry or low humidity environment
- Emotional stress
- Exposure to certain chemicals (e.g. soaps, detergents, perfumes, or cosmetics), materials (e.g. wool or synthetic fibres), dust, sand and smoke
- Food (eggs, peanuts, soy milk)
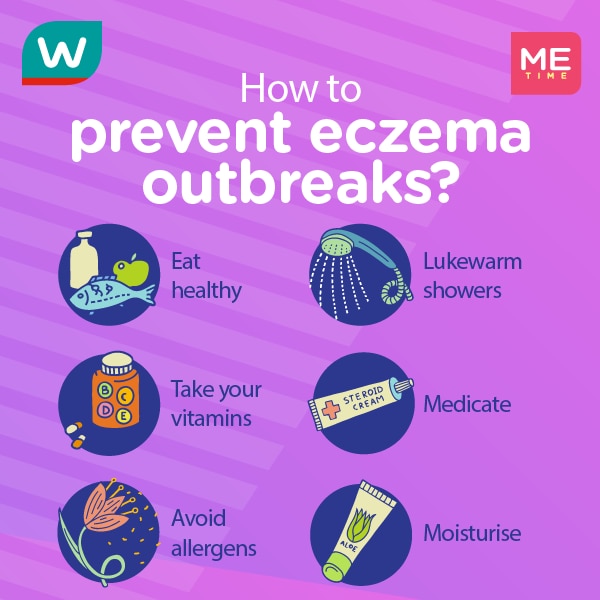
How to prevent Eczema outbreaks?
You can relieve the symptoms with moisturizers, self-care measures and medications. Below are some non-drug measures and mainstay treatments that may help prevent eczema flare-ups:
Scroll to read the treatment and management tips below.
1. Apply moisturizers regularly
Constant hydration with moisturizers is essential in preventing dryness. It also helps to repair the skin barrier and acts as a barrier to external irritants. Their effect is short-lived. So you should apply moisturizer frequently and continuously even when the symptoms have been controlled.
For best results, apply straight after showering. While lotion contains more water than cream and ointment, and is thus easier and more convenient for application, cream and ointment provide longer-lasting hydration to the skin.
The choice of appropriate moisturizer depends on the severity of eczema, individual preference and the site of application. Take short showers or baths (5-15 minutes) using lukewarm water and mild, unscented soap-free cleanser. Gently pat the skin dry with a soft towel after washing it off.
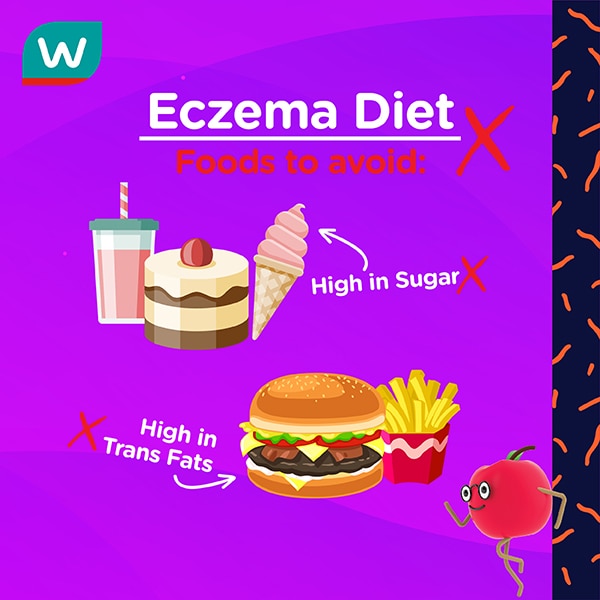
2. Avoid & eat these foods if you have Eczema
3. Turn to topical & oral Medications
During an eczema flare-up, you may use topical steroids to reduce the inflammation and itch. As for the appropriate strength, you should consult your pharmacist or doctor to avoid side effects such as skin thinning
Apply a thin layer adequately to treat the affected area once or twice daily as advised by your pharmacist/doctor.

- Non-steroidal over-the-counter products such as coal tar preparation are available for managing the itch.
- Oral anti-histamines may be taken to relieve the itch. Speak to your pharmacist on selecting the most suitable medication for your condition.
- Topical immunomodulators (medications which act on the immune system) such as tacrolimus* have been demonstrated to be viable options for patients with mild to severe cases of atopic dermatitis.
* Prescription-only medicine
*Disclaimer: please consult your physician for personalized medical advice. Always seek the advice of a physician or other qualified healthcare provider with any questions regarding a medical condition.